(Maram El Sabri,PhD candidate at the University of South Australia)
Pancreatic cancer is highly aggressive and malignant, ranking as the seventh leading cause of cancer-related deaths globally(1). In 2020, it was the 12th most common cancer worldwide, with over 495,000 new cases and 466,000 deaths (accounting for 4.5% of all cancer-related deaths) (1). The survival rates for pancreatic cancer are notably low, with a global five-year relative survival rate of only 9% (2). The disease is categorised into four stages, ranging from I to IV: Stage I (localized and resectable) involves cancer limited to the pancreas, either < 2 cm (IA) or > 2 cm and < 4 cm (IB). Stage II (locally spread or borderline resectable) includes tumours> 4 cm confined to the pancreas or with local spread to nearby lymph nodes. Stage III (wider spread or unresectable) suggests possible involvement with nearby blood vessels or nerves, though no distant metastasis has occurred. In Stage IV (metastatic), cancer has spread to distant organs(2). Unfortunately, due to the asymptomatic nature of early stages, up to 80% of patients are diagnosed at advanced stages (III or IV), contributing to the challenging treatment landscape and the low survival rate(2). Treatment approaches include surgery, radio- and chemotherapy, with the goal of extending survival and alleviating symptoms. However, patients diagnosed at late stages (III or IV) currently lack curative options. This emphasises the urgent need for further research and innovative treatment strategies to address this issue.
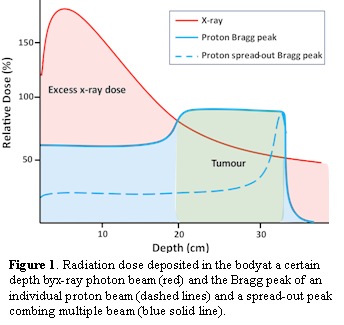
Radiotherapy has evolved significantly in treating pancreatic cancer in past few years, driven by advances in computational modelling and medical imaging(3). The therapeutic index of radiotherapy in pancreatic cancer is narrow, and even minor deviations in treatment plans can have a substantial impact on patient outcomes(3). Challenges arise from the pancreas’ critical location, necessitating careful consideration of normal tissue toxicity, particularly in the gastrointestinal tract. Organs such as the duodenum, jejunum, and stomach are radiosensitive, making careful dosage planning essential(4). Proton radiotherapy, which uses accelerated hydrogen atom nuclei, has been pursued to improve the therapeutic ratio for pancreatic cancer(5). Proton radiotherapy has unique characteristics (Bragg peak) that enable focused delivery of radiation dose to the target while minimising radiation dose deposition to surrounding normal tissue (Figure 1). Dosimetric studies, single-institutional retrospective series, and single-arm prospective studies have shown that proton radiotherapy combined with chemotherapy is well-tolerated and allows for dose escalation(5). Continued trials and advancements in proton planning and delivery techniques are expected to unlock proton radiotherapy’s full potential for treating pancreatic cancer.
To forge a more optimistic future for pancreatic cancer patients, future studies and clinical trials should focus on neoadjuvant therapeutic strategies, novel radiation delivery techniques, and improved patient selection. As radiation therapy advances, it holds greater potential to enhance outcomes in this devastating malignancy.
References:
- World Cancer Research Fund International (WCRFI). Pancreatic cancer statistics: WCRFI; 2022 [2 August 2023]. Available from: https://www.wcrf.org/cancer-trends/pancreatic-cancer-statistics/.
- Rawla P, Sunkara T, Gaduputi V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World journal of oncology. 2019;10(1):10-27.
- Hall WA, Goodman KA. Radiation therapy for pancreatic adenocarcinoma, a treatment option that must be considered in the management of a devastating malignancy. Radiat Oncol. 2019;14(114):1-5.
- Yalamanchili A, Thomas TO, Dajani S, Hayes JP. Evolution of Radiation Therapy in Pancreas Cancer Management toward MRI-Guided Adaptive Radiation Therapy. Journal of clinical medicine. 2022;11(5380):1-12.
- Rutenberg MS, Nichols RC. Proton beam radiotherapy for pancreas cancer. J Gastrointest Oncol. 2020;11(1):166-175.